Introduction: Living with diabetes brings about a unique set of challenges, one of which is an increased susceptibility to opportunistic infections. Among these, cellulitis, a bacterial skin infection, stands out as a common concern for individuals with diabetes. In this blog post, we delve into the intricacies of cellulitis, exploring its causes, symptoms, and crucial preventive measures that can make a significant difference in the lives of those managing diabetes.
What is Cellulitis? Cellulitis is a bacterial skin infection that can affect individuals of all ages, but it poses a particular threat to those with diabetes. Typically caused by bacteria such as Staphylococcus and Streptococcus, cellulitis occurs when these pathogens enter the skin through cracks, cuts, or other openings.
Why Diabetics are at Risk:
- Compromised Immune Function: Diabetes weakens the immune system, reducing the body’s ability to fend off infections effectively.
- Peripheral Neuropathy: Nerve damage, common in diabetes, can lead to decreased sensation in the extremities, making it easier for skin injuries to go unnoticed.
- Poor Circulation: Impaired blood flow hinders the delivery of immune cells to the affected areas, delaying the body’s natural healing process.
Symptoms of Cellulitis:

- Redness and Swelling: The infected area appears red, swollen, and may feel warm to the touch.
- Pain and Tenderness: Discomfort or pain in the affected region, often worsening over time.
- Fever and Chills: Systemic symptoms may include fever and chills, indicating a more severe infection.
Preventive Measures:
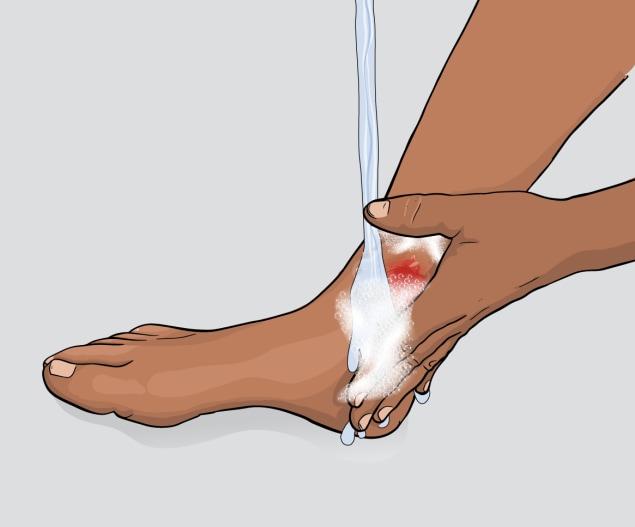
- Maintain Good Hygiene: Regularly clean and moisturize the skin to prevent cracks and breaks.
- Prompt Wound Care: Attend to cuts, scrapes, or injuries immediately to prevent bacterial entry.
- Control Blood Sugar Levels: Proper diabetes management helps reduce the risk of infections.
- Foot Care: Diabetics should pay special attention to foot hygiene and promptly address any foot injuries.
Medical Intervention:
- Timely Antibiotics: If cellulitis is suspected, seek medical attention promptly. Antibiotics are often prescribed to treat the infection.
- Elevation and Rest: Elevating the affected limb and getting adequate rest can aid in the recovery process.
- Follow-up Care: Regular follow-up appointments with healthcare providers are crucial to monitor progress and prevent recurrence.
Conclusion: Cellulitis is a serious concern for individuals with diabetes, but with proper education and proactive measures, its impact can be mitigated. By understanding the risks, recognizing symptoms, and taking preventive actions, those living with diabetes can empower themselves to maintain healthier skin and overall well-being.
Remember, when in doubt, it’s always best to consult with healthcare professionals for personalized advice and guidance tailored to individual health needs.



